The resurgence of ADCs in cancer therapy
The World ADC conference is the leading conference for those working in the antibody-drug conjugate (ADC) therapy industry. World ADC hosted more than 1,200 delegates in San Diego the week of November 4—doubling last year’s attendance.
Riding the recent wave of practice changing clinical results like we’ve seen with Enhertu® in breast cancer and Padcev® in bladder cancer, ADCs are experiencing a resurgence in oncology drug development. The following are some of my key takeaways from the World ADC conference, focusing specifically on the Clinical Lessons track.
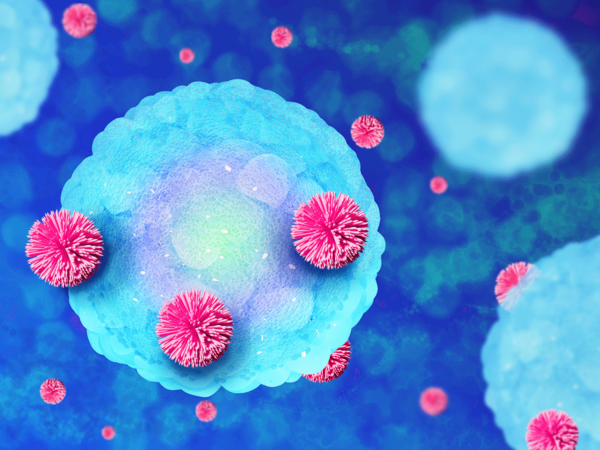
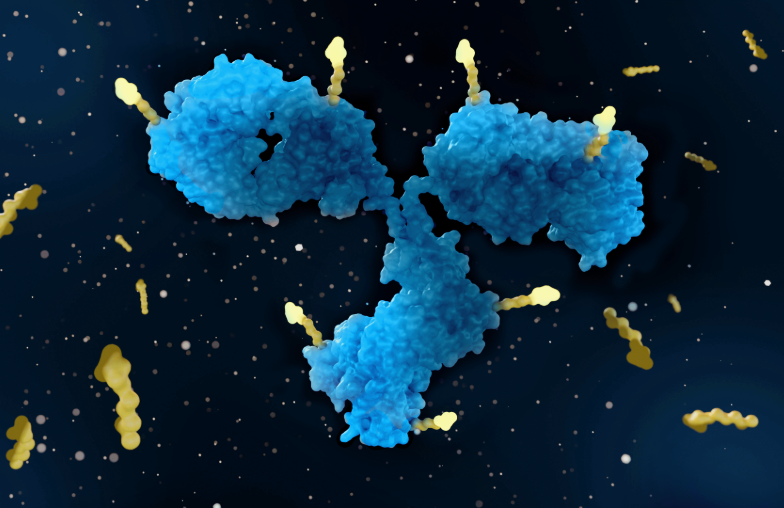
What are ADCs?
ADCs are a type of precision medicine that leverage the targeting ability of monoclonal antibodies. To date, ADCs have focused primarily on delivering cytotoxic drugs (the payload) directly to cancer cells at a concentration that would otherwise be too toxic to dose systemically. ADCs attach to specific proteins (antigens) on the cancer cell and get internalized into the cell. This process cleaves the “linker” to release the payload, delivering treatment directly to the cell and minimizing damage to nearby healthy cells. Through October 2024, fifteen ADCs have been approved globally, and trial starts have increased an average of 22% annually over the last five years.
Improving the safety and toxicity profile of ADCs
A major topic of discussion at this year’s World ADC conference was how to increase efficacy while limiting toxicity. Many first-generation ADCs on the market have known, unique toxicity profiles with the most common being ocular toxicity. These can include corneal pseudomicrocysts, conjunctivitis and keratopathy. The exact mechanism behind ADC-induced ocular toxicity is unknown, but theories include linker instability, bystander effect (discussed below), and direct corneal cytotoxicity of specific payloads. As a result, researchers are exploring different linker technologies and payloads that can be used with the antibodies to reduce the risk of ocular toxicity in patients.
Another poorly understood but highly prevalent toxicity of ADCs is interstitial lung disease (ILD). Characterized by inflammation and scarring of lung tissue, ILD can make it difficult to breathe and can be fatal in severe cases. Recent data suggest this manifests via Fcγ-receptor-mediated uptake by macrophages in the lung, leading to local inflammation, though other theories exist around mechanisms similar to what are thought to cause ocular toxicity. As a result, drug developers are heavily focused on next-generation antibody, linker, and payload design to help lower the risk of ILD toxicity.
The bystander effect
Significant attention at World ADC was garnered by the bystander effect. ADCs are designed to specifically kill cancer cells that express the target antigen, and you want a linker that properly holds onto its payload to help minimize off-target effects. That said, solid tumors are heterogeneous and not all cancer cells express a target antigen at the same level. If the payload is designed to be highly permeable, once it is freed from its linker within the cancer cell, the drug can diffuse to other nearby cells, even those that lack the specific antigen being targeted.
Through a combination of linker, payload, and antibody design techniques, ADC researchers are investigating how to optimize the Bystander Effect given its ability to treat surrounding cancer cells that do not express the same target antigen.
Exploring new technologies for patient screening
With precision medicine like ADCs, oncologists can tailor cancer treatment to an individual’s unique genetic profile. To be effective, however, we must optimize ways to identify patients who are ideal matches for these tailored therapies.
One traditional method used for patient screening for ADCs is the immunohistochemistry (IHC) assay. IHC is a widely used, somewhat qualitative measurement to detect the expression of certain biomarkers on the surface of tumor cells.
There was much discussion at World ADC about the use of IHC for patient screening as it requires a biopsy sample, often freshly obtained, which is a painful, invasive procedure for patients, and not always viable if the tumor is inaccessible. A major topic was the need for new patient screening technology that can provide more precise measurement of biomarker expression or can do so without the need for a biopsy. Circulating tumor DNA is one mechanism being explored that just requires a blood sample, and computational pathology, such as quantitative continuous scoring (QCS). This is a more quantitative approach than IHC and was shown at the recent World Conference on Lung Cancer to predict clinical outcomes in patients with lung cancer treated with a TROP2 ADC.
Combination therapies and the merging of ADCs and radiopharmaceuticals
ADCs have shown significant clinical benefit as a monotherapy. As drug developers look for ways to optimize their effectiveness, they are also beginning to explore how ADCs can be combined with other therapies for enhanced efficacy.
One area of promise being discussed at World ADC is the merging of ADCs and radiopharmaceutical therapies11. With this approach, antibodies are being used to deliver radiation directly to a tumor. This dual approach provides a two-for-one punch with the ADC delivering the cytotoxic payload to kill the cancer cells and the radioactive isotope providing localized radiation to cause further damage to the tumor.
Leveraging ADCs in earlier lines of therapy
In their search to optimize ADC therapy, researchers have also shifted their focus to explore how ADCs can be used in earlier lines of therapy. The U.S. Food and Drug Administration’s (FDA’s) recent approval of Padcev® in combination with pembrolizumab (Keytruda) for the first line treatment of locally advanced or metastatic urothelial cancer, is one such example. The results of the EV-302 study as presented at ESMO last year immediately changed standard of care, showing a nearly doubling of overall survival versus chemotherapy (16.1 months to 31.5 months). Full FDA approval was granted only five weeks after that data was presented. This new area of focus aligns with the FDA’s Project FrontRunner initiative which encourages researchers to investigate new cancer therapies in patients who have not yet undergone multiple lines of treatment, and thereby provide earlier access to potentially life-saving therapies.
World ADC 2024 offered an extremely informative conference on the trends and challenges of ADC therapies. ADCs have taken their seat at the forefront of oncology research, and the future of ADC therapy is indeed promising.
We can help
With our exclusive biotech focus and next-gen oncology experience, Catalyst Oncology supports early- to late-phase drug development across a range of both solid and hematologic indications. Learn about our specialized expertise in managing global ADC trials or connect with us to discover how we can support your ADC therapy development.